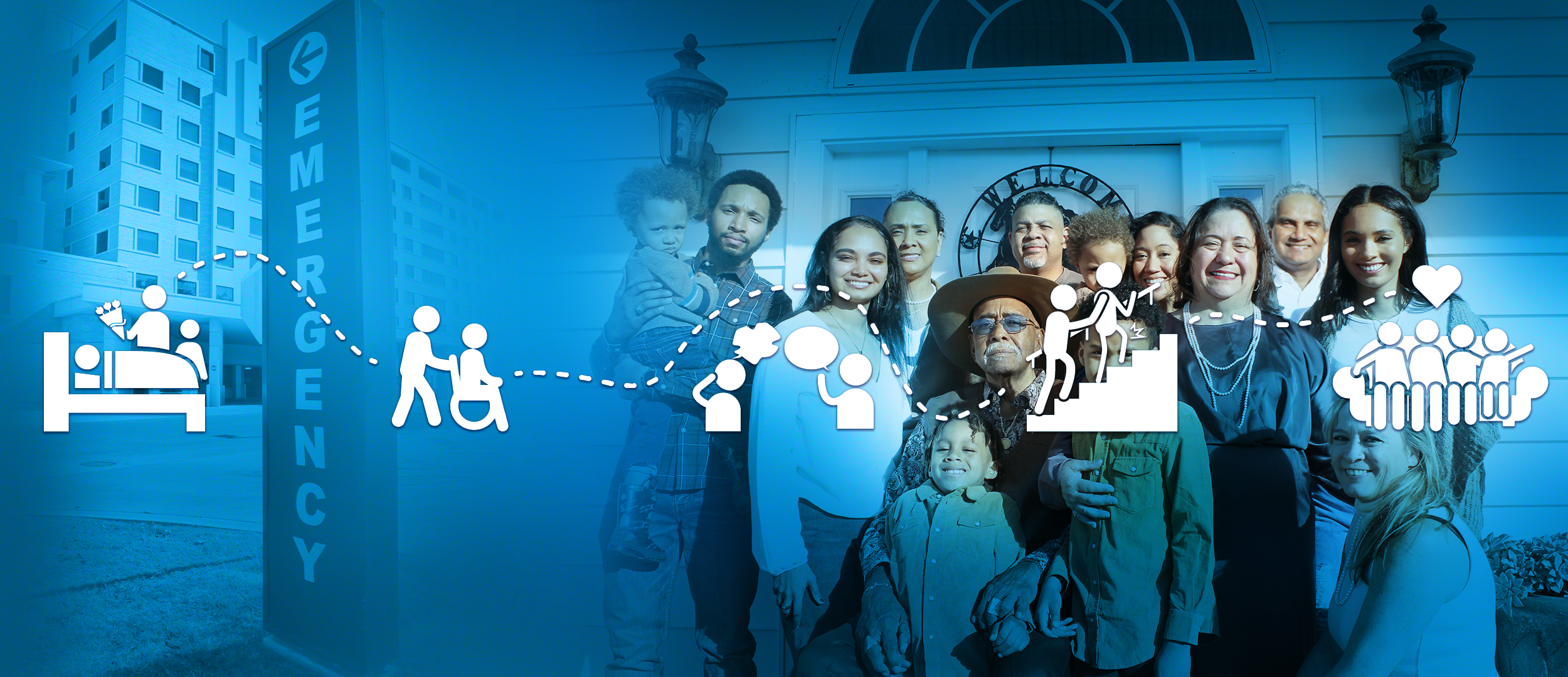
Shared decision-making –
a patient’s perspective
32-year-old Jessica is diagnosed with breast cancer. Her 3-year-old daughter, Laura, is at that delightful chatty age, full of questions. The oncologist tells Jessica that she can have surgery and is given the option of additionally receiving adjuvant chemotherapy. The chemotherapy will eradicate microscopic foci of cancer cells missed in the surgery that could become metastatic cancer. Jessica is warned about the cognitive effects of chemotherapy and ‘chemo brain’ and she worries about how she will be there for Laura. Her oncologist also tells her that chemotherapy could impact her fertility. Laura may never have a brother or sister to play with.
In recent years, ‘the doctor knows best’ method of treatment decision making has been replaced with shared decision making (SDM), where the physician helps the patient to make decisions about their treatment.1 Patients who are empowered to make decisions about their health that better reflect their personal situation experience better health outcomes including decreased anxiety and quicker recovery times. They also demonstrate increased compliance and adherence to treatments.

Where should I go? The difficulty of choosing the treament that is right for me
Merely a few decades ago, a woman could go in for a breast cancer biopsy and wake up from the procedure to learn that not only did she have breast cancer but that the surgeon had already removed it.
Ensuring that patients understand the pros and cons of their treatment options and that the patient’s goals and personal preferences guide their decision making is no easy undertaking. As in the case of Jessica, treatment decisions are complicated not only by uncertainty about their effectiveness and the balance of benefits and harms, but by the personal implications of the treatment.
It is essential that not only do patients have access to a variety of sources of information including a multidisciplinary team of physicians, nurses and psychologists, but also materials in the form of medical education websites, videos and printed brochures and articles.
Patient materials should explain treatment options without bias, highlighting the pros and cons of each option, and providing support for patients to express their personal goals and preferences. They can be used by HCPs before, during and after visits.2
We at infill understand that visual information increases both a patient’s understanding and the retention of information. We recognise that written materials must be both understandable and contextual. We have a dedicated team of medical writers and designers who work together to prepare easily accessible content across a broad range of medical conditions for both pharma and patient advocacy groups.
If you are you interested in preparing patient materials, please contact us at info@infill.com.
References
- Muscat, D.M. et al.Health Literacy and Shared Decision-making: Exploring the Relationship to Enable Meaningful Patient Engagement in Healthcare. J GEN INTERN MED 2021: 36;521–524.
- Strategy 6I: Shared Decisionmaking. Content last reviewed March 2020. Agency for Healthcare Research and Quality, Rockville, MD.
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html